Athlete's Foot
What is Athletes Foot? Athlete's foot is a fungal infection of the feet and is highly contagious. The skin becomes dry, flaky and itchy. If left untreated, may lead to blisters and cracks that can be painful and particularly itchy.
Known as tinea pedis, athletes foot thrives in dark, moist and warm conditions such as inside your shoe - especially if you have sweaty feet in close fitting socks and shoes. Minute fungi grow and multiply on the human skin, particularly the feet. Some people are more prone to this condition while others are able to resist the condition easily.
The more serious problem is that of the athletes foot infection spreading to the toenails (Onychomycosus). Very common especially in those undertaking distance running. Constant damage to the nails often results in them becoming black or partly falling off. This often leaves a cavity under the toe nail that is very susceptible to becoming infected with the surrounding athletes foot, turning the nail a brownish yellow colour. If not treated this may spread to other nails and unfortunately remains as a reservoir for the continued re infection of athletes foot to the rest of the feet.
Symptoms, Causes, & Treatment

Athlete’s foot is a contagious fungal infection that occurs on the feet, usually between the toes (typically the fourth and fifth toes), on the soles, or on the sides of the foot. It can cause the feet to itch, burn, and become dry and flaky, and can cause discomfort as the condition spreads and worsens over time. Athlete’s foot is medically known as tinea pedis, or ringworm of the feet. Athlete’s foot is so named because many sufferers are athletes, who spent a lot of their time sweating and going into public showers, gyms, locker rooms, and other damp, warm places. But you don’t have to be an athlete to suffer from athlete’s foot. Fungi thrive in warm, damp places. Our shoes are a perfect example. During warmer weather, podiatrists see an increase in athlete’s foot.
Athlete’s Foot Symptoms To Pay Attention To
Athlete’s foot is said by sufferers to begin with a mild itching sensation. As the condition persists, scales begin to form in the same area. The scales are usually soft, moist, and either red or grayish-white in colour.
In most cases they begin to form around the toes, but they have also been known to appear on the sides of the feet, on the heels, or on the soles. Occasionally blisters develop on the feet. Some athlete’s foot sufferers say their feet smell damp and mouldy.
Seek advice immediately if you are experiencing these symptoms, which may be signs the infection is spreading:

Athlete’s foot can sometimes spread to the hands and face, but these cases are extremely rare. Diabetics need to be extremely aware of the health of their feet. If you have diabetes and contract athlete’s foot, you should discuss it with your podiatrist.
Why Do I Have Athlete’s Foot?
This condition is usually caused by a fungal infection, which is spread by direct contact with someone who is already infected. Athlete’s foot can also be caused by:


All the items listed above increase the risk for developing athlete’s foot. For example, if you don’t regularly wash your feet with soap and water, or if you do not wash your socks every time you wear them, you are at a higher risk for developing athlete’s foot. Also, if you frequent public places that require you to be barefoot even for a moment—for example, if you change in a public changing room or use a public shower—you are increasing your chances of developing this condition.
Additional risks that may increase your chances of contracting athlete’s foot include:
Diagnosing Athlete’s Foot
Most people can diagnose themselves with athlete’s foot, if you are not sure discuss it with your pharmacist, podiatrist or GP. Sometimes the problem may not respond to treatment or keep reoccurring. If this occurs we will probably take samples of the scales to test in a laboratory to rule out other skin conditions. We should then be able to diagnose you properly upon examining your skin sample.
The tests may include one or more of the following:
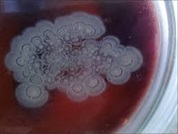
- Skin Culture
We take samples of fungi and skin from the patient and grow them in their lab. - A positive microscopy or a positive culture of skin scrapings is recommended before starting treatment
If test results are negative but the clinical appearance is very suggestive of fungal infection, a repeat sample will be taken and treatment started. - Skin Lesion Biopsy
A small sample of skin is taken and examined under a microscope. - PCR (polymerase chain reaction)
Testing is both the most sensitive and most specific method to diagnose dermatophyte infections and eventually will become the gold standard for diagnosing such infections.

How Is Athlete’s Foot Prevented?
There are several things you can do to prevent athlete’s foot from occurring:


How Is Athlete’s Foot Treated?
What over-the-counter product can be used for mild athletes foot?
Complications of Athlete’s Foot That May Develop

There are a few complications that may arise if you suffer from this condition, including:


