Stress Fractures
Stress fractures usually affect people who have suddenly increased their activity levels, whether it be that they’ve taken up a new sport or have suddenly increased their training levels, be it the intensity, duration or frequency.
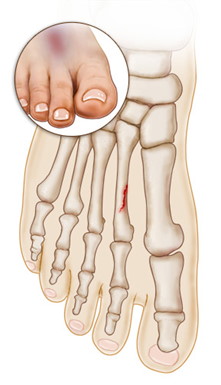
Stress fractures are the result of repeated application of stress to the bones—hence the name. Our feet, which hold all of our body weight, are under continuous stress every day, making them particularly susceptible to this type of injury. Stress fractures are sometimes described as small cracks or hairline fractures in the bone.
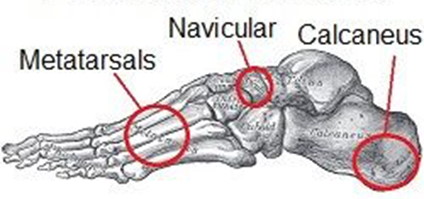
Stress fractures can occur in any bone in our bodies, but our feet are the most common location. This type of fracture can happen to any of the foot bones but it mainly occurs in the second and third metatarsal bones, in the navicular bone and in the calcaneus (heel bone).

Our muscles act as shock absorbers. When they are fatigued or overloaded, they cannot absorb the shock and stress of repeated impacts, and end up transferring the stress to nearby bones. Over time, the bones begin to weaken and become prone to fractures and cracks. Athletes of all kinds are susceptible to this injury, but runners seem to be more prone than other groups.
Women seem to be at greater risk of foot-stress fractures than men due to a condition called “the female athlete triad,” which is a combination of inadequate nutrition, disrupted or irregular menstrual cycles and a resulting reduction in bone density. This condition is known to weaken the bones and therefore results in an increased risk of stress fractures in the feet. As well as athletes, women after menopause are more susceptible to osteoporosis and other diseases that weaken bones and can often develop multiple stress fractures.

There are a few symptoms to watch for if you think you may have a stress fracture in your foot:

You should be able to wiggle your toes and move your foot and ankle around with a stress fracture injury to the foot. Many people believe stress fractures immobilize sufferers, and when they are not immobilized, they fail to take the injury seriously enough to seek treatment.
Many runners who have suffered stress fractures say they did not realize the seriousness of the problem until the pain was unbearable. They would run on their injured foot for months, before seeking medical attention. Many sufferers are fooled when their pain diminishes after they exercise.
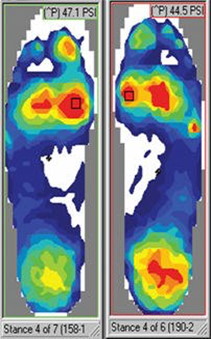
Stress fractures are caused by repetitive impacts sustained over time, combined with fatigued muscles that become unable to absorb the stress and shock of each impact. However, there are other factors, such as how often you exercise (or how often you rest!), how long you exercise, and your level of exercise intensity.
All these affect how much stress you put on your lower leg muscles and feet. You do not have to be athletic to suffer a stress fracture in your foot.
Post-menopausal women are more susceptible to osteopaenia and osteoporosis and other diseases that weaken bones.
Even normal household activities can create stress fractures.
Other causes of stress fractures in the foot include:

If you suspect you have a stress fracture in your foot or ankle, you should avoid walking on the injured area.
Do not ignore the pain, especially if it is coupled with the symptoms listed previously.
If you try to walk on the foot or ignore the symptoms, you could break your bone completely. Instead, apply an ice pack and elevate your foot at least as high as your hip. If possible, take ibuprofen to relieve the pain and swelling (this may not help at all if the injury is severe).
But please note, be aware of the risks involved with taking NSAID (nonsteroidal anti-inflammatory drug) like ibuprofen in a situation like this, as such drugs may inhibit bone healing. If the fracture is caught early, as with all injuries, the damage may be minor and easily treated.

A detailed medical history will be taken to identify predisposing factors, as well as review of any recent change of activity or increase in use to help evaluate your risk of stress fractures.

A thorough examination of the area will take place to rule out other problems that cause similar symptoms.
To get a better understanding of what is happening inside your foot, imaging tests may be necessary.
An MRI scan can detect a stress fracture in its early stages, even before an X-ray, however X-rays will often be taken first.
MRI scans are more sensitive than x-rays, which can only detect stress fractures after the healing process has begun.

Most stress fractures happen to active people. Stress fractures need plenty of time and rest to heal. Healing is delayed and prevented by continued weight applied to the fracture during the healing process.
Treat the area with the RICE method.
When you have a stress fracture, appropriate first aid can help minimize inflammation and prevent further injury.
The most effective form of first aid for a stress fracture is the RICE (Rest, Ice, Compression, Elevation) protocol. Immediately after you are injured and while you are waiting to get medical care, do the following:

- Rest your injured foot as much as possible. If you must walk around or put weight on your foot, wear a supportive shoe (such as a sandal with a thick, cork sole).
- Ice your foot. Apply an ice pack to the injured area for 20 minutes at a time, with 20-minute breaks in between. Wrap the ice pack with a tea towel to protect your skin.
- Compress the area with a tubegrip bandage to reduce swelling.
- Elevate your foot, keeping it above the level of your hip. Try lying down on a couch with your foot propped up on the armrest, or lying in bed with your foot propped on a couple of pillows.

Your healing time will depend on the severity of the fracture, the location, your body’s ability to heal, your dietary habits and ability to rest the foot. Once the stress fracture heals and you are pain-free, you will slowly be able to resume your activities. In most cases, recovery takes four to six weeks of rest and immobility.
Crutches, walking boots, and casts are used to prevent a patient from putting weight on the injury. Patients are advised to keep weight off the foot at all times. In severe cases, surgery may be necessary to ensure that the bones heal properly, and a wheelchair may be required.
This could lengthen recovery time up to eight weeks or more, depending on the severity of the injury and the type of treatment needed.
IMPORTANT : Stress fractures in the foot tend to begin healing rather quickly, and symptoms diminish. This prompts some patients to resume normal activities too soon, before the stress fracture has actually healed. This can result in delayed healing and could possibly worsen the problem. Always consult your doctor about changes in your condition, even improvements.

