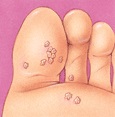
Verrucie or Plantar Warts
Warts are one of several soft tissue conditions of the foot that can be quite painful. They are caused by a virus, which generally invades the skin through small or invisible cuts and abrasions. They can appear anywhere on the skin, but technically only those on the sole are properly called plantar warts.
Children, especially teenagers, tend to be more susceptible to warts than adults; some people seem to be immune.
Symptons
Most warts are harmless, even though they may be painful. They are often mistaken for corns or calluses—which are layers of dead skin that build up to protect an area which is being continuously irritated. The wart, however, is a viral infection.
It is also possible for a variety of more serious lesions to appear on the foot, including malignant lesions such as carcinomas and melanomas. Although rare, these conditions can sometimes be misidentified as a wart. It is wise to consult a podiatrist when any suspicious growth or eruption is detected on the skin of the foot in order to ensure a correct diagnosis.
Plantar warts tend to be hard and flat, with a rough surface and well-defined boundaries; warts are generally raised and fleshier when they appear on the top of the foot or on the toes. Plantar warts are often gray or brown (but the color may vary), with a center that appears as one or more pinpoints of black. It is important to note that warts can be very resistant to treatment and have a tendency to reoccur.
Source of the Virus
The plantar wart is often contracted by walking barefoot on dirty surfaces or littered ground where the virus is lurking. The causative virus thrives in warm, moist environments, making infection a common occurrence in communal bathing facilities.
If left untreated, warts can grow to an inch or more in circumference and can spread into clusters of several warts; these are often called mosaic warts. Like any other infectious lesion, plantar warts are spread by touching, scratching, or even by contact with skin shed from another wart. The wart may also bleed, another route for spreading.
Occasionally, warts can spontaneously disappear after a short time, and, just as frequently, they can recur in the same location.
When plantar warts develop on the weight-bearing areas of the foot—the ball of the foot, or the heel, for example—they can be the source of sharp, burning pain. Pain occurs when weight is brought to bear directly on the wart, although pressure on the side of a wart can create equally intense pain.
Prevention
It is not easy to prevent athlete's foot because it is usually contracted in dressing rooms, showers, and swimming pool locker rooms where bare feet come in contact with the fungus. However, you can do much to prevent infection by practicing good foot hygiene. Daily washing of the feet with soap and water; drying carefully, especially between the toes; and changing shoes and hose regularly to decrease moisture, help prevent the fungus from infecting the feet. Also helpful is daily use of a quality foot powder.
Tips
- Avoid walking barefoot, except on sandy beaches.
- Use flip flopps in the showers.
- Change shoes and socks daily.
- Keep feet clean and dry.
- Check children's feet periodically.
- Avoid direct contact with warts—from other persons or from other parts of the body.
- Do not ignore growths on, or changes in, your skin.
Home treatment
Treatment for children is usually not difficult for 9 out of 10 children. Preparations from the pharmacy containing about 25 % salicylic acid will often be successful in treating verrucie when smaller than a pea or less than 5 in number. Often treatment must be applied daily for up to six weeks. is generally not advisable. Over-the-counter preparations contain acids or chemicals that destroy skin cells, and it takes an expert to destroy abnormal skin cells (warts) without also destroying surrounding healthy tissue. Self treatment with such medications especially should be avoided by people with diabetes and those with cardiovascular or circulatory disorders. Never use them in the presence of an active infection.
Professional treatment
It is possible that your Podiatrist will prescribe and supervise your use of a wart-removal preparation. More likely, however, removal of warts by a simple surgical procedure, performed under local anesthetic, may be indicated.
Cryosurgery
Freezing warts with liquid nitrogen is a popular treatment. Liquid nitrogen is sprayed on, or applied to, the wart. Liquid nitrogen is very cold and the freezing and thawing destroys the wart tissue. To clear the wart fully it usually needs 3-5 treatments, a couple or weeks or so apart. The chance of clearing a wart with freezing treatment is about the same as acid treatment. However, it is quicker. Freezing treatment can be painful. Sometimes a small blister develops for a day or so on the nearby skin after treatment. Also, there is a slight risk of scarring the nearby skin or nail, or damaging underlying tissues such as tendons or nerves. It is not suitable for younger children or for people with poor circulation.
Dry needling
What is dry needling?
Dry needling is a proceedure where the verruca / wart is punctured with a small needle to cause bleeding and stimulate the body’s immune system to resolve the problem.
Is it painful?
This procedure is performed under local anaesthetic and therefore does not hurt. A recent study found that patients experienced minimal post operative pain.
What is the advantage of this procedure?
There are many treatments for a verruca / wart although the results are mixed and the treatments are often painful. In addition, they often require several consultations.
Dry needling is an effective treatment, often working following the first treatment. Patients can remove the dressing the next day and continue as normal.
Is this suitable for multiple / large verrucae/ warts?
The treatment is appropriate for all verrucae / warts although often the largest is targteetted in the first instance?
If it does not work, what are my options?
The treatment can be repeated but any of the other common treatments can still be provided.
Will I need to take a pain killer afterwards?
These are generally not necessary and anti-inflammatories should be avoided as there is a theoretical chance this could reduce the body’s immune response to the treatment.
How successful is the treatment?
Until recently, there was very little information on success rates. However, a recent paper has demonstrated:
- 31 patients (69%) had complete resolution
- 3 patients had reduced size and pain
- 11 showed no improvement
- There were no post operative infections or scarring
- Only mild symptoms were reported – bruising, slight discomfort
The paper is available at: Dry Needling
